Part 3: Fundamental Mistakes Healthcare Providers Make With Deaf and Hard of Hearing Individuals
Part 1 of the Series
Part 2 of the Series
—
In the first two parts of this series, I discussed the importance of providing Deaf awareness, cultural and sensitivity training to hospital employees, as well as the significance of working with reliable, reputable interpreting and captioning agencies to ensure effective communication is provided. In this third and last part of this series, I discuss the erroneous assumption that video remote interpreting (VRI) is the all-encompassing solution for sign language interpreting services.
Assuming VRI results in effective communication
When you go to the doctor’s office, you expect board certified doctors. You expect the same thing when using a doctor via video.
Would you still use a video platform to access medical care if doctors via video were not board certified?
In a state like Illinois, on-site interpreters in medical settings must have specific credentials (e.g., national certification). However, if you put an on-site interpreter in a different room than the patient and give them a computer or tablet with a webcam and speaker, the legal requirements (e.g., minimum credentials and/or certifications) for interpreters go away. Simply put, there are no minimal standards enforced for video interpreting in Illinois and many other states.
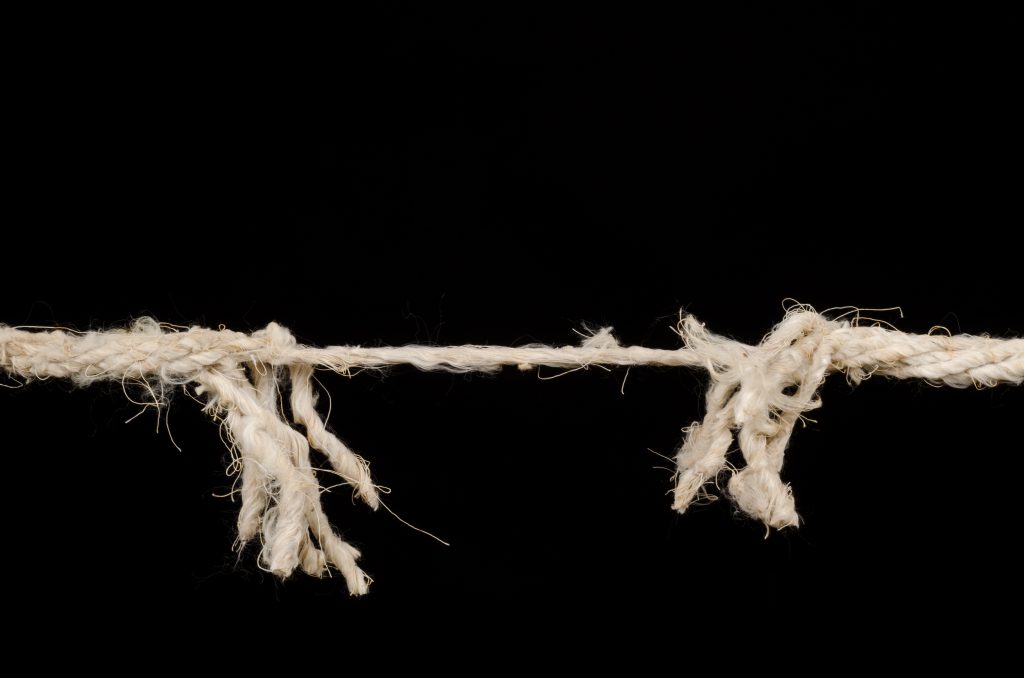
While the courts have decided the effective use of video remote interpreting (VRI) technology requires the technology to be in excellent working order, it is also important to consider concerns posed by using non-certified or appropriately trained interpreters via VRI.
The ADA emphasizes clear communication in health care settings is critical to avoid “misdiagnosis and improper or delayed medical treatment.” To this end, as the National Association of the Deaf discuss in their position statement regarding minimum standards for VRI services in Medical Settings, a video interpreter shall “accurately, effectively, and impartially interpret all communications between the deaf and hard of hearing patient and/or companion and the medical provider staff/contracting medical personnel.”
While there are some VRI providers who require their interpreters to have national certification and specialized training, Deaf and Hard of Hearing individuals remain at risk of lower communication access standards in states like Illinois.
Similar to depending on unqualified on-site interpreters, depending on unqualified VRI interpreters may impact hospitals’ bottom lines. Hospitals may suffer from reduced throughput, decreased efficiency and increased patient re-admissions (the latter will cost the hospital more money to provide interpreting or captioning services each time a patient is re-admitted). Furthermore, hospitals may subject themselves to litigation for not providing effective communication.
At the end of the day, it is hospitals’ responsibilities to ensure the services and aids provided result in effective communication. This puts the burden on hospitals to screen VRI providers to ensure their interpreters are qualified and competent.
Recommended Next Steps
At a fraction of the costs associated with a settlement agreement or judgment in favor of the plaintiffs, 2axend can provide a wide range of training and consultation services to help your organization improve the overall experiences of Deaf and Hard of Hearing individuals.
Contact us today – we’re ready to help you stay compliant, reduce risk and protect your reputation.