Do Lawsuits and Patient-Centric Healthcare Experiences Align?
This post was co-authored by Isabelle Garreaud, legal research intern at 2axend, and Corey Axelrod, founder and CEO of 2axend.
—
Steve Breyer was unable to take care of his dying mother.
Kathryn Arcana and Peggy Merhi were excluded from participating in decision-making while their young son was in the hospital.
Dawn Siegel was unable to communicate with her doctors after being admitted to a hospital and having unexpected surgery.
These are the names of several individuals who recently sued healthcare providers for failing to provide effective communication in healthcare settings. Unfortunately, these stories are commonplace for Deaf and hard of hearing individuals and leave them feeling frustrated, scared, and even traumatized.
How is this patient-centered?
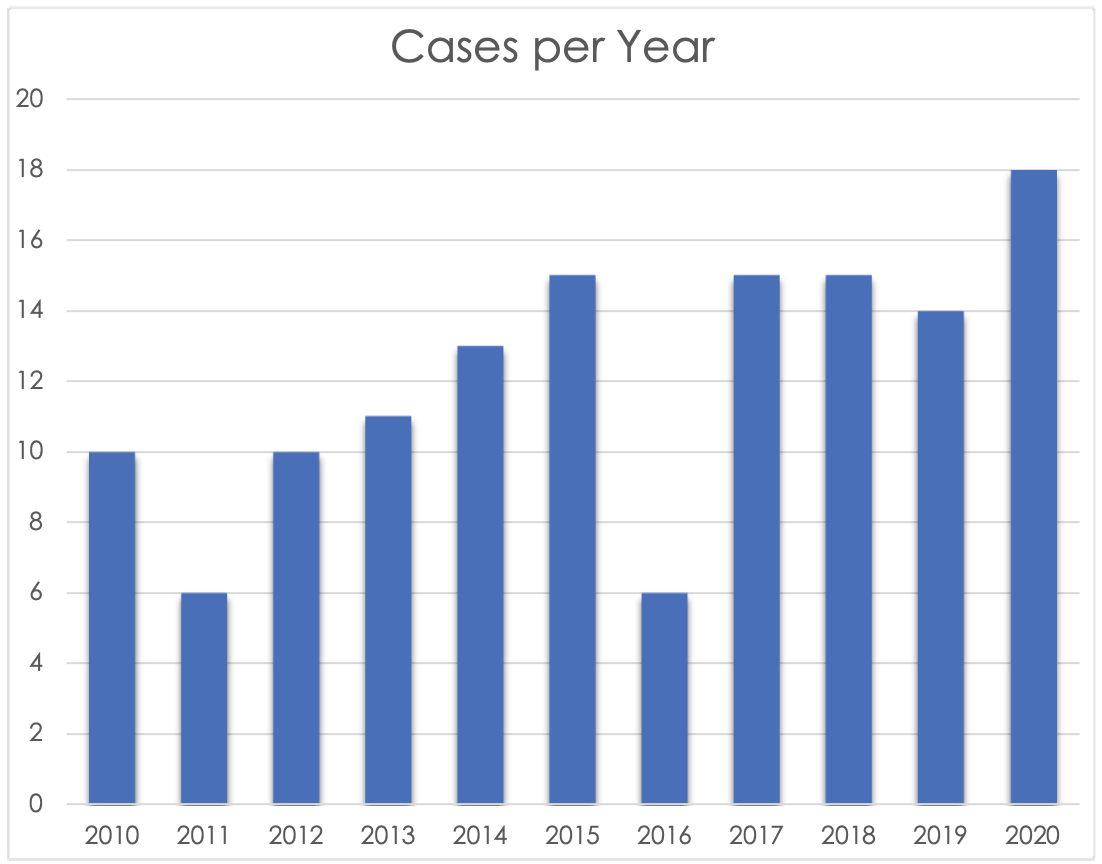
Upon an in-depth search of healthcare-related lawsuits involving Deaf and hard of hearing plaintiffs, we found 135 cases that were finalized over the past ten years. While a considerable figure, this number does not include private settlements, recently filed lawsuits, and the numerous complaints that did not make its way into the legal system.
Within our research, we found an increase of lawsuits filed after the Barrier-Free Healthcare Initiative was established in 2012 by the Department of Justice. Through this initiative, there was an increased emphasis on U.S. Attorneys’ offices across the nation and the DOJ’s Civil Rights Division ensuring people with disabilities have access to medical services and facilities. These targeted enforcement efforts included Deaf and hard of hearing individuals having access to effective communication.
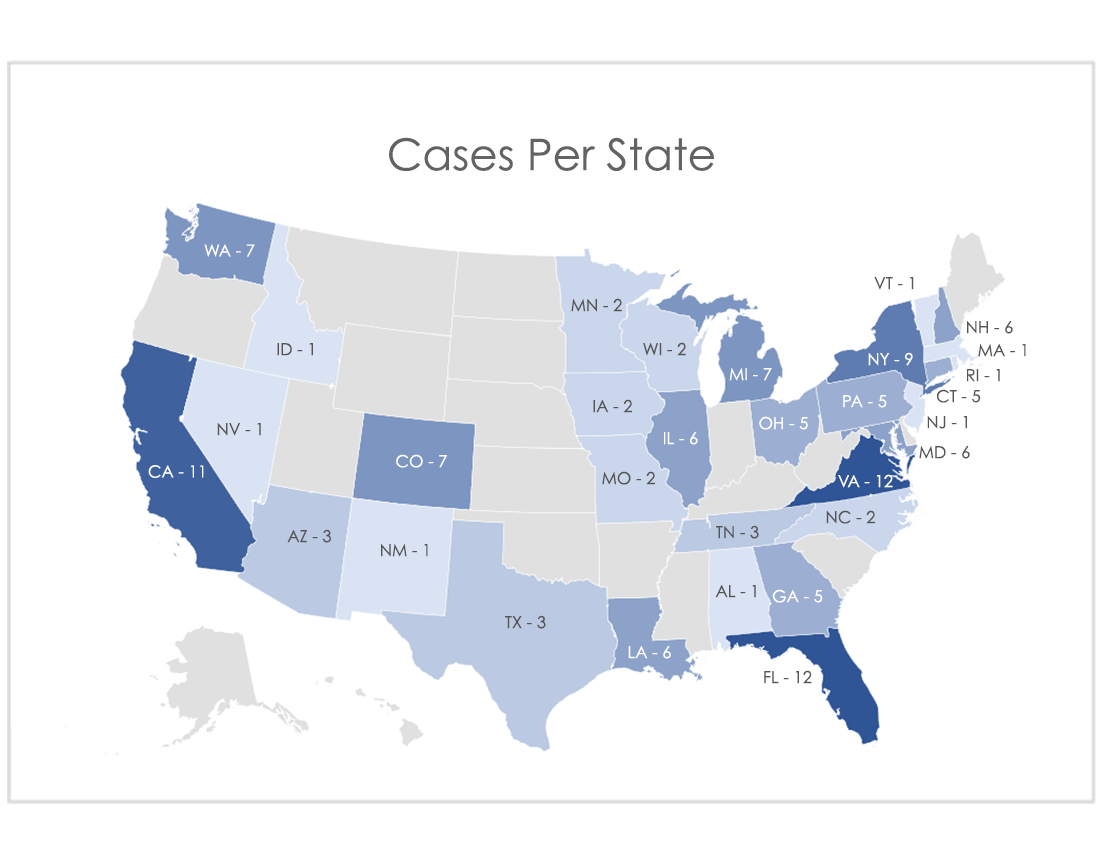
The cases we found spanned 31 states. 71 percent of these suits were filed against hospitals and more than half of these hospitals were non-profit. Each of these cases featured similar stories of patients and companions being denied in-person sign language interpreters and other appropriate auxiliary aids and services that are listed in Section 504 of the 1973 Rehabilitation Act (Section 504), the Americans with Disabilities Act (ADA), and other civil rights laws.
Additionally, with respect to the denial of in-person sign language interpreters, providing video remote interpreting (VRI) as the sole auxiliary aid for Deaf and hard of hearing individuals was documented as one of the chief complaints in more than 20 percent of the cases we researched. VRI is an on-demand service that uses videoconferencing technology, equipment and a high-speed Internet connection to access an off-site interpreter that provides real-time sign language interpreting services for conversations between hearing and Deaf/hard of hearing individuals. These complaints were heavily rooted in the failures and limitations of VRI, including issues with the technology, equipment and bandwidth, all of which we’ll delve further in this summative assessment of cases.
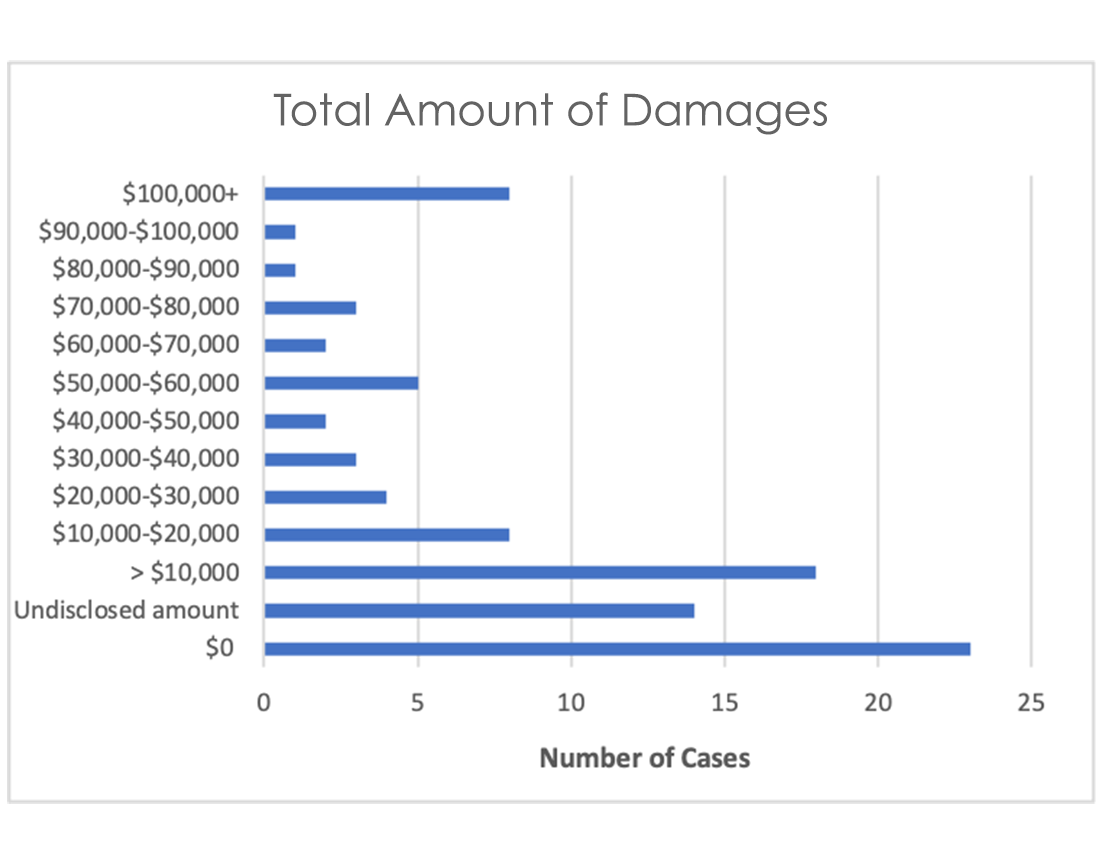
While the majority of the cases were settled before going to trial, disclosed awarded damages ranged between $500-353,000 (not including attorney fees, if awarded) and averaged $46,929 per case. Damages were also granted to friends and family members, including children, who were forced to act as an interpreter for the Deaf or hard of hearing individual. Each of the cases that settled, including 23 cases that had no damages, or were decided in favor of the plaintiff required that healthcare providers take corrective action to address issues with the provision of auxiliary aids and services.
Furthermore, in 20 cases in which the USA, via the Department of Justice, was the leading plaintiff, the healthcare organization had to pay a civil penalty to the government ranging from $1,000 to $75,000. The ADA states that the maximum penalty for a first violation is $55,000 and a maximum of $110,000 for every subsequent violation.
Alternatively, cases that were decided in favor of the healthcare organization or provider often highlighted the limitations of Section 504 and the ADA.
In a 2014 lawsuit, Hayes v. San Fernando Community Hospital, the defendant argued that the plaintiff could do without an interpreter while hospitalized due to being able to text and email on his phone, as well as maintaining employment without using an interpreter. The jury’s verdict was in favor of the defendant.
In another case in favor of the defendant, Nash v. Medina, the plaintiff asserted that the defendant’s refusal to provide medical services to her was because she was Deaf and required an interpreter. The defendant argued the undue hardship clause of the ADA on two primary contentions: 1) the interpreter costs would have exceeded the insurance reimbursement for treating the plaintiff and 2) the defendant’s practice was small and they had difficulty meeting expenses.
Regardless of the outcomes of the aforementioned cases, it is prudent to recognize the impact of these disparate experiences on Deaf and hard of hearing individuals.
A lack of meaningful and effective communication between providers and patients can decrease patient satisfaction and the quality of care. [1] [2] [3] [4] This can result in misdiagnosis, increased readmissions, decreased throughput, unwanted procedures and surgeries, and, in some cases, life-threatening mistakes.
In another case we reviewed, Dykman v. Bowden, M.D., a DeafBlind individual sued her ophthalmologist for denying her an interpreter. The miscommunication resulted in a failure to obtain informed consent and unwanted surgeries on her left eye; yet, the jury’s verdict was in favor of the defendant.
Earlier this year, a Deaf couple filed a complaint, Miller v. Christ Hospital, stating they were not given the appropriate auxiliary aids and services on multiple occasions. One such incident where no interpreter was provided led to Mrs. Miller being misdiagnosed with a urinary tract infection, which turned out to be a fibroid that needed to be surgically removed. This case ended with a private settlement.
TraciAnn Hoglind founded the non-profit organization, Health Signs Center, Inc., with the goal of making health-related information and resources linguistically and culturally accessible to the greater Deaf, hard of hearing, and DeafBlind community. In an article she wrote that is published on the Boston University School of Public Health’s website, Hoglind shared that after being denied an interpreter during a doctor’s visit and visibly noticing her doctor’s uncomfortableness with communicating with a Deaf patient, she was prescribed the wrong medication and subsequently suffered from pneumonia for two weeks before going to the hospital for an emergency antibiotic IV.
These encounters collectively underscore the need for healthcare providers to not only provide effective communication but also drive optimal experiences for Deaf and hard of hearing individuals throughout the entire care continuum. However, the continued prominence of these cases being filed only further exacerbate the disproportionate health inequities encountered by Deaf and hard of hearing individuals.
Andrew Montoya, Legal Program Attorney at Colorado Cross-Disability Coalition who has represented Deaf and hard of hearing individuals in approximately 10 healthcare-related cases, shared, “Although we are more than 30 years after the ADA was signed into law, far too many individuals and entities still seek to place the onus of communication access on the Deaf and hard of hearing individual despite the ADA and its implementing regulations’ remarkable clarity on this issue.”
Montoya touches on a prevalent issue: healthcare providers not understanding their legal obligations to provide patients with effective communication. These issues were at the forefront of various cases we researched, including a recently settled case this year in California, USA v. Dr. Javier Rios, where the plaintiff was told her insurance was the one responsible for obtaining the interpreter, not the doctor’s office. In another case that was settled with remedial action, USA v. Bhupinder S. Mangat, M.D. & Seminole Neurology Associates, P.A, a Deaf woman told the doctor’s office that pursuant to the ADA, they were required to get her an interpreter. The Deaf woman was told no and hung up on. Another case that settled with remedial actions, USA v. The Heart Center of Memphis, involved a Deaf patient trying to get an appointment with a cardiologist but was told by staff that it was the patient’s responsibility to hire an interpreter.
Another common challenge Deaf and hard of hearing individuals face is healthcare providers doing what is perceived as the bare minimum by attempting to communicate via handwritten notes or VRI. As these often do not position communication for successful interactions, this approach can be attributed to civil rights laws providing minimum baseline requirements with subjective language.
In the case of Rosario v. St. Tammany Parish Hospital Service District No. 1, the defendant effectively argued they attempted to communicate and were in legal compliance. The plaintiff was 32 weeks pregnant at the time of the alleged discrimination and, during a routine visit, was instructed by her obstetrician to go to the emergency room. Throughout her hospital stay, the healthcare team communicated with the plaintiff via handwritten notes and VRI. Eventually, after repeated requests, one of the nurses called an interpreter referral agency and was informed that there were no interpreters available. Despite misunderstandings taking place due to ineffective communication, the defendant was granted a motion for summary judgment, as the judge determined the plaintiff was unable to prove that the hospital intentionally discriminated against her by not providing an in-person interpreter.
We also connected with Matthew Dietz, litigation director of Disability Independence Group in Florida, to discuss his experience in representing Deaf and hard of hearing individuals in more than 75 cases where they were allegedly denied the appropriate auxiliary aids and services. When we asked Dietz what he wants healthcare providers to understand, he succinctly stated, “VRI is not always effective.” In 2018, Dietz was part of the court of appeals legal team for Sunderland v. Bethesda Health, a case that included 9 Deaf patients and the Florida Association of the Deaf as plaintiffs. The complaints arose after Bethesda Hospital switched from live-interpreters to VRI and advised patients that they were required to pay for an in-person interpreter if they did not want to use VRI. The United States Court of Appeals for the Eleventh Circuit reversed the District Court’s judgment and provided the plaintiffs with monetary damages and injunctive relief.
It is rather disconcerting that a number of healthcare providers have chosen VRI as the sole auxiliary aid to provide Deaf and hard of hearing individuals. Two other cases where the challenges of VRI were documented as the chief complaint, USA v. Riverside Medical Clinic, Inc. and Esparza v. University Medical Center Corporation, were also recently settled. While Dietz was not involved with these cases, they further illustrate the prominence of challenges Deaf and hard of hearing individuals face when using VRI.
In response to these ongoing issues with VRI, the National Association of the Deaf and Deaf Seniors of America collaboratively drafted a position statement on minimum standards for video remote interpreting services in medical settings. In this position statement, they discussed the controversial increased use of VRI in medical settings, assessing Deaf and hard of hearing individuals’ communication needs as a means of determining how to best provide effective communication, as well as the need to use VRI as a last resort.
Furthermore, Dr. Kushnalgar and her colleagues published “Video Remote Interpreting Technology in Health Care: Cross-Sectional Study of Deaf Patients’ Experiences” in the Journal of Medical Internet Research (JMIR). Dr. Kushnalgar, the director of the Center for Deaf Health Equity at Gallaudet University, is the principal investigator of National Institute of Health (NIH) awards that total over $3 million dollars. These grants support studies aligned with her primary research interests in deaf patient-reported and health outcomes. In the JMIR-published study, they found only 41 percent of Deaf and hard of hearing individuals surveyed were satisfied with the quality of the VRI technology service.
While it remains to be seen the long-term impacts of these collective pieces of work, it is also critical to emphasize the importance of healthcare organizations receiving training on effective communication and Deaf culture. This is a topic we explored in depth with Dietz and Bill Richards, another attorney committed to changing hospitals’ practices one lawsuit at a time.
Richards, owner of Richards & Moskowitz PLC, has represented more than 100 Deaf and hard of hearing individuals, with a vast majority of lawsuits being filed against healthcare providers. During a conversation with Richards, he shared among the most appalling conduct he has come across in his work was healthcare personnel comparing Deaf and hard of hearing patients to incapacitated patients unable to participate in their own care. As these professionals used this justification for not providing sign language interpreters, this further illustrates the need for healthcare organizations to receive adequate training on how to best work with Deaf and hard of hearing patients.
To this end, Richards shared, “The big dilemma in healthcare is keeping people sensitized and trained and having someone at the hospital whose job includes making sure that every new person that comes in the door knows how to work with interpreters and knows how to identify and get the help their Deaf and Hard of Hearing patients need.”
We also connected with Marissa Rivera, the daughter of two Deaf parents and advocate at Disability Rights Connecticut (DRCT). DRCT is a non-profit organization that was founded in 2017 to provide legal advocacy and rights protection to those with disabilities. During an email exchange with Rivera, she shared that DRCT receives a minimum of five calls a year from Deaf and hard of hearing community members regarding healthcare inaccessibility. She described these calls as “consistent” and that they necessitate the need for systemic change rather than addressing the issues on a case-by-case basis.
With healthcare moving towards a model focused on cultivating relationships based on trust and loyalty, the emphasis should no longer be solely on mitigating risk exposure and enhancing organizational compliance. Healthcare organizations should employ strategies and initiatives to promote effective Deaf and hard of hearing patient and provider interactions as this will improve patients’ outcomes and reduce the health disparities the Deaf and hard of hearing community experiences.
At 2axend, we strongly believe Deaf and hard of hearing individuals cannot continue to be left out of healthcare organizations’ commitment to provide the best care for everyone who walks through their doors. As part of our ongoing #DeafInHealthcare campaign aimed to raise awareness of the ongoing issues in healthcare settings, we created a self-assessment tool for healthcare organizations to help them assess their capacity to satisfy Deaf and hard of hearing individuals’ cultural, social, and linguistic needs in clinical settings.
As a starting point, healthcare organizations understanding their respective shortcomings and areas of opportunities is of utmost importance. This will only help drive patient-centric experiences and advance the quality, safety, and care for Deaf and hard of hearing individuals, as well as ensure encounters like the ones Breyer, Arcana, Merhi, Siegel, and countless others have experienced will diminish.
—
Resources/References
[1] Barnett S, Klein J, Pollard Jr R, Samar V, Schlehofer D, Starr M, Sutter E, Yang H, Pearson T. Community Participatory Research With Deaf Sign Language Users to Identify Health Inequities. Am J Public Health. 2011;101(12):2235-2237.
[2] McKee M, Barnett S, Block R, Pearson T. Impact of Communication on Preventive Services Among Deaf American Sign Language Users. Am J Prev Med. 2011;41(1):75-79.
[3] McKee M, Moreland C, Atcherson SR, Zazove P. Hearing Loss: Communicating With the Patient Who Is Deaf or Hard of Hearing. FP Essent. 2015 Jul;434:24-8. PMID: 26161525.
[4] Moreland, C., Atcherson, S.R., Zazove, P., & McKee, M.M. (2015). Hearing loss: Issues in the Deaf and Hard of Hearing communities. FP Essentials, 434, 29-40.